Biomedical Science and Research Journals | Epidemiological Characteristics and Management of Brain Metastases on Patients in the Clinical Hospital of the University of Chile (Hcuch) between 2012 and 2017
Epidemiological Characteristics and Management of Brain Metastases on Patients in the Clinical Hospital of the University of Chile (Hcuch) between 2012 and 2017
Abstract
Introduction and Context: Brain metastases (BM) are the main neurological complication of cancer, affecting up to 30% of these patients (incidence = 8.3-14.3 x 100,000), and they are the most frequent intracranial tumors (IT) of the adult. They are 10 times more common than primary cerebral neoplasms (PCN), however, the number of publications about this pathology is only 25% of PCNs such as gliomas. In our country there is no national registry of brain tumors, so the actual incidence of these is unknown. Treatments include initial/palliative management with glucocorticoids (GC) and/or surgery (Cx), radiosurgery (RS) or Whole Brain Radiation Therapy (WBRT). The purpose of this study is to determine clinical and therapeutic characteristics of BM in patients taken care of in our institution and with this information we propose the improvement of the management of these patients.Material and Methods: In this cohort study we analyze the clinical records of patients treated in our hospital during the years 2012-2017 with a diagnosis of BM. The date of death was obtained from the National Identification Registry and Identification Service and calculated the median survival between diagnosis and death. We registered: sex, age at diagnosis, number of brain metastases, management and survival rate.
Results: 54 CR were found with a diagnosis of BM, however, only 31 complied with Inclusion criteria (IC). Average age at diagnosis of symptomatic BM: 59 years (range: 29-86 years), men (n=13): 56.3 years and in women (n=18): 60.9 years. BM number: 14 patients (45,1%) had one BM; 11 (35,5%) had oligometastases (2 or 3); and 6 (19,4%) patients multiple BM (more than 3). Origin of primary tumor: 45.2% pulmonary; 12.9% colorectal; 12.9% renal; 9.7% breast; 3.2% ovary; 3.2% unknown; 12.9% other (Includes gastric, hepatic and thyroid). Only 38.7% of BM had BB, 25% were poorly differentiated lung carcinoma, 16.7% colon adenocarcinoma and 16.7% moderate/poorly differentiated breast carcinoma. Clinical Features (CF) highlights includes motor symptoms and signs in 54,8%, headache in 48,4% and gait apraxia in 38,7%. Location: 67.7% of patients had hemispheric tumors and 35.5% cerebellar. There were no brainstem tumors in our study. 12 (38.7%) patient received active treatment (surgery or radiosurgery),11 (35.5%) had surgery and only one (3.2%) received radiosurgery. All patients received palliative care, and 10 received WBRT. Survival: one patient was alive. For those who had a certified death, average survival time after diagnosis was 34.9 weeks (N=30). People who received active treatment, had an average survival time of 56.1 weeks after diagnosis and 54.5 weeks after treatment (N=12). Patients which did not receive an active treatment (N=18) had an average survival of 20.7 weeks. The hazard rates differ between those who had an active treatment and those who did not (log-rank test), z test = 2.25, p = 0.0246).The survival -in weeks- of patients who WBRT (N=10) versus those that were only managed with palliative care (GC) (N=8) was z test = 2.76, p = 0.00578. In the group of people who received active treatment, there was no difference between the ones that had unique BM vs those with 2 or 3 BM. In the group that received active treatment, 3(25%) patients died because of their BM but there was no difference with the palliative group.
Conclusion: BM is a prevalent oncological complication. The age of presentation is primarily between 4th-7th decade of life, the main primary tumor comes from lung, and the main location is at the frontal lobe. All patients should be given palliative treatment and active treatments are offered to selected patients with better prognosis. The average survival for patients with active treatment in our institution is 54.5 weeks better than the WBRT and palliative group.
Keywords: Cancer; Brain metastases; Brain radiotherapy; Palliative care
Abbreviations: PCN: Primary Cerebral Neoplasms; BM: Brain Metastases; IT: Intracranial Tumors; CNS: Central Nervous System; CF: Clinical Features; GC: Glucocorticoids; SRS: Stereotactic Radiosurgery; WBRT: Whole Brain Radiation Therapy; CR: Clinical Records; IC: Inclusion Criteria; BB: Brain Biopsies; EC: Exclusion Criteria
Introduction
Brain metastases (BM) is the main direct neurological complication of cancer and the most frequent intracranial tumors (IT) in adults [1]. They are ten times more frequent than primary cerebral neoplasms (PCN) and its current management involves mostly palliative therapy but is at this moment evolving towards an active therapy either by surgical means or radiosurgery, which has shown a better prognosis [2]. The number of published papers on BM only achieves 25% of gliomas [3]. Metastases to Central Nervous System (CNS) are common, affect 30% of patients with cancer [4]. BM are the most frequent expression of intracranial malignancy with an incidence varying between 8.3 and 14.3 per 100,000 [5]. However, are not the intracranial tumors most frequently operated, it is estimated that around 20-25% of BMs have a surgical indication. The candidates for surgery are patients with best prognostic factors, such as: age, controlled systemic disease, good functional status (Karnofsky), usually single and localized in non-eloquent area. The cause of death of these patients is in most cases due to metastatic disease and only 25% die of neurological causes [6]. In our country there is no national registry of brain tumors, so the actual incidence of these is unknown [7]. 80% of CNS metastases are in the hemispheres, particularly in the territory of the middle cerebral artery and the posterior cerebral artery. In descending order: frontal, parietal, temporal and occipital [8]. The origin of BM highlights lung cancer, following with lower percentages breast cancer and melanoma [9]. BM are more frequent between the fifth and seventh decade of life and 75% of patients have multiple metastatic tumors [10]. The clinical features (CF) are varied, including headache as an initial symptom in 50% of patients [11]. Treatments include: initial/palliative management with glucocorticoids (GC) and/or surgery (Cx), stereotactic radiosurgery (SRS) or Whole Brain Radiation Therapy (WBRT) [6].Objective
To study and describe epidemiological and clinical-therapeutic characteristics of BM patients in the Clinical Hospital of the University of Chile (HCUCH).Methodology
This is a cohort study of a cross-section period between 2012 and 2017. The information was obtained from clinical records (CR) of patients treated at the HCUCH. Inclusion criteria (IC) and exclusion criteria (EC) were defined based on the available clinical records:IC: adult patients diagnosed with BM during 2012-2017.
EC: incomplete registry and/or diagnostic doubt between primary brain neoplasm and BM.
The following data was registered: sex, age at diagnosis, BM number, clinical features, primary cancer, clinical status, management and outcome. We also reviewed reports of pathological anatomy of existing brain biopsies (BB) of patients who met the IC. The cause and date of death was obtained from the death certificates of the National Identification Registry and CR. Survival was estimated from the date of imagenologic diagnosis to the date of death for all patients. Subsequently, the information was analyzed, and the Kaplan-Meier survival curves were configured using the Log-Rank Test, comparing survival rates between active vs non-active treatment. Significance was established when p < 0.05. This report was approved by the ethics committee from HCUCH.
Results
54 CR were found with a diagnosis of BM, however, only 31
complied with IC (Graph 1). Average age at diagnosis of symptomatic
BM: 59 years (range: 29-86 years), men (n=13): 56.3 years and in
women (n=18): 60.9 years (Graph 2). BM number (Graph 3): 14
patients (45,1%) had one BM; 11 (35,5%) had oligometastases (2
or 3); and 6 (19,4%) patients multiple BM (more than 3). Origin of
primary tumor: 45.2% pulmonary; 12.9% colorectal; 12.9% renal;
9.7% breast; 3.2% ovary; 3.2% unknown; 12.9% other (Includes
gastric, hepatic and thyroid) (Graph 4). Only 38.7% of BM had
BB, 25% were poorly differentiated lung carcinoma, 16.7% colon
adenocarcinoma and 16.7% moderate/poorly differentiated breast carcinoma (Graph 5). Clinical Features (CF) highlights includes
motor symptoms and signs in 54,8%, headache in 48,4% and
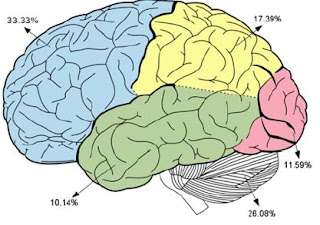
gait apraxia in 38,7% (Table 1). Location: 67.7% of patients had
hemispheric tumors and 35.5% cerebellar (Figure 1). There were
no brainstem tumors in our study. 12 (38.7%) patients received
active treatment (surgery or radiosurgery),11 (35.5%) had surgery:
tumor resection including one ventricular peritoneal shunt and
only one (3.2%) treated with radiosurgery. All patients received
palliative care, and 10 received WBRT.Survival: One patient is still alive. For those who had a certified
death, average survival time after diagnosis was 34.9 weeks (N=30).
People who received active treatment, had an average survival
time of 56.1 weeks after diagnosis and 54.5 weeks after treatment
(N=12). Patients which did not receive an active treatment (N=18)
had an average survival of 20.7 weeks. The hazard rates differ
between those who had an active treatment and those who did not
(log-rank test), z test = 2.25, p = 0.0246).The survival in weeks of
patients who WBRT (N=10) versus those that were only managed
with palliative care (GC) (N=8) was z test = 2.76, p = 0.00578 (Graph 6). In the group of people who received active treatment, there was
no difference between the ones that had unique BM vs those with
2 or 3 BM (Graph 7). Cause of death: In the group that received
active treatment, 3 (25%) patients died because of their BM but
there was no difference with the palliative grow. Future Proposals:
Improvements to this project could include a multicentric analysis
and a more thorough.
Discussion
There are few Chilean studies about BM [2,12] In this study the age of presentation is mainly between 50 and 70 years (59.4%), including an important group of patients who were reported in their 4th decade of life (22.6%). Also 45.1% of patients had a single BM, 35.5% oligometastases and 19.4% of patients emerged with multiple BM, incidence that has not been reported as in other studies [10]. According to previous reports the leading origin of primary tumor was pulmonary (45.2%), but our breast incidence (9.7%) was lower than other reports and colorectal and renal (12.9%) were higher. None of our patients was reported with melanoma. A major group displayed hemispheric tumors (frontal, parietal, occipital, temporal) followed by a significant pool of cerebellar tumors, as in other papers [10]. The clinical presentation coincides with the literature including headache in nearly 50% of patients, and an important group with motor symptoms and signs (54.8%) and gait apraxia (38.7%). Cognitive impairment was found only in the group >50 years. may be because of there were only three frontal BM with mild symptoms and also gait ataxia was not found because of less posterior fossa oligometastases.According with other studies [13] 25% of our patients with active treatment died because of neurological associated causes. It is important to consider that only patients in good functional status and with a small number and size of BM were candidates to active treatment. There was a significant difference in survival between patients who received active treatment and the group treated with palliative management (p<0.05). This result supports the active management in selected patients [12,14]. In our country radiosurgery is not available for all patients that is the reason for only one patient treated. There was also a significant difference when we compared WBRT versus palliative management. This has been reported in the literature since several years [15].
Conclusion
Brain Metastases are an important oncologic complication. As
in other studies, we found that the average age of presentation is in
between the fourth and seventh decade of life, also that pulmonary
cancer is the main primary on these patients and the main location
for these metastases is the frontal lobe. Palliative care is mandatory
for all these patients, but active management must be given to
selected patients with a better prognosis. All patients should be
discussed in the neuro-oncological committee to evaluate the
possibility for an active treatment such as surgical or radio surgical
treatment. Future Proposals: Improvements to this project could
include a multicentric analysis
To view fulltext of article:https://biomedgrid.com/fulltext/volume2/epidemiological-characteristics-and-management-of-brain-metastases-on-patients.000608.php
For More information: biomedical open access Journals: https://biomedgrid.com/index.p
Open Access Journal of Biomedical Science and Research
Know More Information: Biomed Grid Please Click on : https://biomedgrid.com

Comments
Post a Comment