Biomedical Science and Research Journals | Hepatic Adenomas Challenges to their Diagnosis and Management with Emphasis on the Bordeaux Classification
Hepatic Adenomas Challenges to their Diagnosis and Management with Emphasis on the Bordeaux Classification
Goals and Learning Objectives
a. To discuss the etiology and natural history of HA.
b. To detail the importance of the Bordeaux Classification.
c. To provide a comprehensive approach to their correct identification based on imaging and pathological features.
d. To present the risk factors associate with hepatic carcinogenesis.
e. To elaborate on the entity of hepatic adenomatosis.
f. To detail on the state-of-the-art management of HA and adenomatosis.
g. To emphasize their association to congenital cardiac conditions and other syndromes.
Disclosure Statement
Authors have nothing to disclose.
Etiology and Natural History of Hepatic Adenomas (Ha)
It has been postulated that disrupted hepatic vasculature results in the development of hepatic lesions including hepatic adenomas, FNH, and hemangiomas. The etiology of HA is that an altered hepatic circulation stimulates the evolution of hepatic adenomas, FNH and hemangiomas. The stimuli provided by estrogen and anabolic steroids in the genesis of HA is well established and first recognized by Edmundson. They can result from abnormal carbohydrate metabolism such as: in glycogen storage disease, mature onset diabetes mellitus of the young type 3 (MODY3), and metabolic syndrome.
Other factors include
Anabolic steroids exposure, Fanconi Anemia, glycogen storage disease types I, III and IV, and familial adenomatous polyposis.
Risk Factors Associated with Hepatic Carcinogenesis
Hepatocellular Carcinoma (HCC) in HA. Risk factors for malignant transformation of HA include: Male sex, glycogen storage disease and Anabolic steroid usage. B-catenin–mutated subtype (highest risk of malignancy) and tumors larger than 5 cm in maximum dimension. Teaching Point! B-catenin mutated hepatocellular adenomas are interpreted as borderline lesions between hepatocellular adenoma and hepatocellular carcinoma.
Hepatocellular Adenoma: Histology
HA have dilated sinusoids which are thin-walled capillaries that are perfused by arterial pressure; adenomas lack a portal venous supply and are fed solely by peripheral arterial feeding vessels. Because a tumor capsule is usually absent or incomplete, hemorrhage may spread into the liver or abdominal cavity. Billiary ductules are notably absent from adenomas, a key histologic feature that helps distinguish hepatocellular adenoma from focal nodular hyperplasia [1, 4, 3, 4, 5, 6, 7] (Figure 1).
The Bordeaux Classification of Hepatic adenomas represents a multi-center series of 96 liver tumors with a firm or possible diagnosis of HA was reviewed by liver pathologists. This represents a collective experience from 13 French university hospitals encompassing from 1992-2004. All 96 cases were proven HA. Criteria of inclusion in the study had adequate sampling of frozen and fixed liver tissues following hepatectomy (95 cases) or transplantation (1 case). The HA were analyzed and classified according to their genetic profile, pathological and clinical manifestations
HA and Genetic Mutations
Activation of the B-catenin pathway has been found in HA (18-20) and is present in 20 to 34% of hepatocellular carcinomas (21-24). Beta Catenin is key in hepatic physiology: cell lineage and differentiation, stem cell renewal, epithelial-mesenchymal transition, proliferation and cell adhesion (25, 26). Twentytwo (4.5%) patients had HCC transformation. Predictors of HCC transformation, using both univariate and multivariate analyses, were male gender (odds ratio [OR]: 15.0; IC 95%: 5.4 – 44.0) and tumor size >10 cm (OR: 6.9; IC 95%: 2.5 – 20.1).
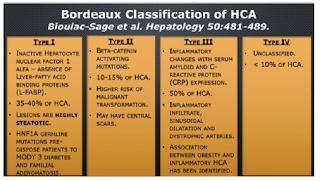
Bordeaux Classification of HCA
Type I
1. Inactive Hepatocyte nuclear factor 1 alfa – absence of Liver-fatty acid binding proteins (L-FABP).
2. 35-40% of HCA.
3. Lesions are highly steatotic.
4. HNF1A germline mutations pre-dispose patients to MODY 3 diabetes and familial adenomatosis.
5. Second most common (30-35%).
6. Associated with maturity-onset diabetes mellitus of the young (MODY3).
7. Predisposition for hepatic adenomatosis.
8. Develop exclusively in female with history of oral contraceptive use.
9. Intracellular fat results in signal loss on out-of-phase MRI– prevalence 86-100% Estrogens in OCP act as the genotoxic agent resulting in somatic mutations of the HNF 1 alpha resulting in lipogenesis and hepatocellular proliferation; the resulting silencing of hepatic fatty acid binding proteins in hepatocytes resulting in intracellular fat deposition (Figure 2).
Type II
1. Beta-catenin activating mutations.
2. 10-15% of HCA.
3. Higher risk of malignant transformation.
4. May have central scars.
5. Prevalence 10-15%.
6. No Specific MRI Patterns.
7. Occur More Frequently in Males, Associated with Hormone Administration, Glycogen Storage Disease and Familial Adenomatosis Polyposis Syndrome.
8. Β-Catenin is encoded in the beta catenin gene (ctnnb1) located in CHROMOSOME 3Q21.
9. It is the downstream effector of the WNT- β-catenin pathway which has a major role in liver embryogenesis [Figure 2].
Adenomas – Management
Surgical due to propensity for bleeding and malignancy.
Lesions > 5 cm; Liver adenomatosis – resection of largest and most vulnerable to hemorrhage (sub-capsular and/or pedunculated), pregnancy and increased risk of hemorrhage [8, 9, 10, 11, 12, 13, 14].
Hepatic Adenomatosis
a) Etiology is poorly understood; described in 1985 by Flejou et al. familial predisposition. Presence of 10 or more HA´s involving both hepatic lobes.
b) Females in their 4-5 decades of life with a 10-24% prevalence. (6). Associated with non-alcoholic fatty liver disease (NASH).
c) Presence of congenital or acquired hepatic vascular abnormalities.
d) All sub-types of HA may be found in hepatic adenomatosis.
e) Elevated serum alkaline phosphatase and gamma glutamyl transferase.
f) Do not respond to withdrawal of steroids.
g) Increased risk for HCC.
h) Monitoring with alfa feto-protein.
i) Resection of larger adenomas.
j) Imaging characteristics of adenomas similar to HA not associated to liver adenomatosis
Conclusion
I. Imaging characteristics play a key role in determine the surveillance and management of hepatocellular adenomas.
II. Inflammatory hepatocellular adenomas demonstrates peripheral dilated sinusoids (A toll sign), these are not associated with malignant differentiation.
III. Hepatocellular adenomas larger than 5 cm has greater risk for hemorrhage and rupture.
IV. Malignant transformation of hepatic adenoma is likely low and has a male predominance.
Over view fulltext of article: https://biomedgrid.com/fulltext/volume6/hepatic-adenomas-challenges-to-their-diagnosis-and-management-with-emphasis.001052.php

Comments
Post a Comment