Biomedical Science and Research Journals | Atrial Autonomic Denervation for The Treatment of Longstanding Symptomatic Sinus Bradycardia: A Case Report
Atrial Autonomic Denervation for The Treatment of Longstanding Symptomatic Sinus Bradycardia: A Case Report
Abstract
A 56-year-old man with symptomatic sinus bradycardia (SB) of 5 years accepted the suggestion of atrial autonomic denervation. Radiofrequency pulses were delivered on atrial ganglionated plexi (GP) with positive vagal reflex according to the standard of heart rate (HR) drop ≥20% after high frequency stimulation (HFS). The endpoint of inexistence of HR decrease at repeating HFS was achieved in 16 sites. After 12 months of follow-up, the patient continued to have normal 24-hour total heart beats and mean heart rate and SB-related symptoms substantially improved. Autonomic denervation in LA and RA by endocardial ablation of GP may increase sinus rate and improve symptoms in non-elderly patients with symptomatic longstanding SB.
Introduction
Sinus bradycardia (SB) is not unusual in non-elderly individuals, most of whom are asymptomatic. Pacemaker implantation has been proven efficient for patients with longstanding symptomatic SB [1,2]. However, subsequent multiple pacemaker replacements impose a relatively high economic burden, and long-term non-physiological pacing might lead to atrial arrhythmia and enlargement [3]. The decision of implanting a pacemaker in a non-elderly patient with an apparently normal heart and symptomatic longstanding SB remains challenging. Lately, radiofrequency (RF) ablation aimed at the atrial areas with autonomic innervation has been considered as new treatment of vasovagal syncope [4-6]. We hypothesized that an autonomic activity imbalance driven by a long-term hyperactivity of the parasympathetic nervous system may underlie SB in selected non-elderly patients, and that endocardial radiofrequency (RF) ablation in GP areas may injure the parasympathetic postganglionic neuronal cells, leading to the increase of sinus rate.
Case Report
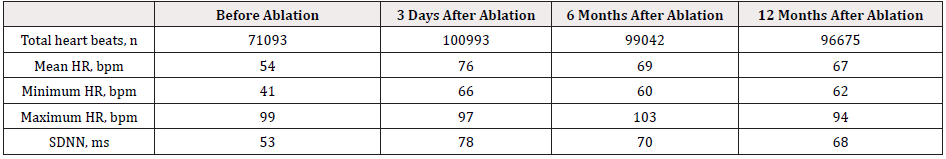
A 56-year-old man presented with symptomatic SB (dizziness and fatigue) of 5 years. Holter monitoring showed a total heart beats of 71093, the mean heart rate (HR) was 54 beats/min (bpm), the minimum HR was 41 bpm and maximum HR was 99 bpm. Echocardiography and coronary angiography demonstrated no evidence of structural heart disease. After the patient refused pacemaker implantation, atrial autonomic denervation using catheter ablation was offered. Before the ablation procedure, atropine test was done by the usual dosage of 0.03 mg/kg (maximum total dose <2 mg) with intravenous injection. During the atropine test, the maximum heart rate was 105 bpm, the HR increase was 55 bpm and time to maximum heart rate was 48s. No supraventricular or ventricular arrhythmias occurred during testing. Ablation was performed after written consent and comprehensive Holter.
Vital signs (HR, oximetry, blood pressure, and respiratory rate) were monitored with a Philips polygraph. One quadripolar electrode catheter was placed in the coronary sinus from the left subclavian vein, and two quadripolar electrode catheters were placed in the His bundle region and the right ventricle from the leftfemoral vein. Sinus and atrioventricular node (AVN) function were analyzed, including corrected sinus node recovery time (cSNRT), atrioventricular node effective refractory period (AVN-ERP) and atrioventricular node Wenckebach conduction time (AVN-Wenckebach). The 3-D geometry of right and left atria (RA and LA) was obtained with a Carto system and a 3.5-mmtip ablation catheter (Navi-StarTM-Thermo CoolTM, Biosense Webster, Diamond Bar, CA, USA). Intravenous heparin was used to maintain activated coagulation time at around 250s. Surface ECG and bipolar endocardial electrograms were continuously monitored and recorded (Cardiolab, Pruka Engineering, USA). Intracardiac electrograms were filtered from 30-500 Hz and measured at a sweep speed of 100 mm/s. Based on the anatomic distribution of GPs, high-frequency stimulation (HFS) following a previously described protocol [7] (20 Hz, 10 mA, 4 ms, MicroPace EPS320, Canterbury, Australia) was applied endocardium to locate major atrial GP based on a positive vagal response. A positive vagal response was defined as a decrease in HR by ≥20% [8].
HFS was delivered to 5 areas with a sequence of right inferoposterior area (inferior right GP-IRGP), left inferoposterior area (inferior left GP-ILGP), left superolateral area (superior left GP-SLGP), right superoanterior area (anterior right GP-ARGP) in LA, and superior vena cava-aorta area (SVC-Ao GP-SAGP) in RA. Irrigated RF current with a power output of 35-40W, maximal temperature settings of 43℃, and 30 seconds was delivered on positive sites. The immediate endpoint of ablation was inexistence of the HR decrease at repeating HFS in each positive site. If one RF pulse of 30 seconds could not reach the endpoint, additional RF pulses with each 20 seconds were delivered until the endpoint was achieved. There were 16 positive sites. Seven sites located in RA, including four sites near the coronary sinus ostium and three sites near the RA close to superior vena cava. The other nine sites were at the posterior wall of the pulmonary vein antrum, including two sites near the left superior pulmonary vein, three sites near the left inferior pulmonary vein, two sites near the right superior pulmonary vein, and two sites near the right inferior pulmonary vein. The endpoint was achieved in all 16 sites and the total time of RF delivery was 560 seconds. During RF delivery to the GP sites, vagal reflex was manifested as sinus rate decrease, sinus pause or junctional rhythm. The time from RF delivery to the minimal HR was 21.1 ± 5.8 seconds; the HR decrease was 33.6 ± 16.7 bpm with the decline rate of 49.8% 23.4%. There were five long intervals (≥3 seconds) with the total time of 22.5 seconds, where one site was in the RA and four sites were in the LA. There were eight bursts of junctional rhythm during ablation, including six bursts in the RA and two bursts in the LA. After finishing the procedure, significant changes were observed in the atrial-His interval (83-63ms), AVN-ERP (442-330ms), Wenckebach cycle length (550-370ms), SNRT (1470-980ms), and cSNRT (420-140ms); however, there was no change in P-A, His-ventricular, and QRS intervals. There were four bursts of atrial fibrillation (AF) and three bursts of atrial tachycardia (ATa) at using HFS to locate the vagal reflexes sites. Both AF and ATa were paroxysmal (lasting 13-372 seconds) and terminated themselves, and no cardioversion was applied.
After the ablation procedure, the patient was hospitalized for 2 days and cardiac rhythm was continuously monitored during the first 48 hours. Holter monitoring was repeated at 3 days, 6 months and 12 months after index procedure, and the outcome was shown in Table 1. HR and heart rate variability (HRV)-related parameters were analyzed from Holter recordings using a commercially available software algorithm. All clinical symptoms including dizziness, fatigue, or palpitation were carefully documented. During the follow-up of 12 months, the patient reported significant symptom improvement, and HR parameters such as total heart beats, and mean and minimum heart rate showed significant increases that persisted for 12 months after the ablation procedure. Compared with before ablation values, time and frequency-domain HRV parameters showed significant decreases that persisted for 12 months after ablation. Inappropriate sinus tachycardia was not observed.
Discussion
Although patients with symptomatic longstanding SB are generally old, a considerable number of these patients are younger, including teenagers, most of whom are completely asymptomatic, and SB is incidentally detected during a routine physical examination or in ECG recording. However, some bradycardia-related symptoms such as dizziness, easy-fatigability and reduced exercise capacity gradually manifest with age in some of these patients. Pacemaker implantation is indicated for non-elderly patients with symptomatic longstanding SB.
However, it may be challenging due to several factors:
- Atropine testing shows negative reaction. SB in non-elderly patients is often not caused by an intrinsic sinus node disease [9]
- Long-term non-physiological pacing may lead to atrial arrhythmia and enlargement,
- Subsequent multiple pacemaker/lead replacements carry a substantial cumulative risk such as lead/pocket revision and infection [10] and
- The cost of these replacement/revision can be substantial as well. Sinus rhythm and rate are regulated by the sympathetic and parasympathetic nervous systems whose elements reside in atrial GP within which parasympathetic postganglionic neuronal cells lie in close proximity to the myocardium [11]. Cardiac autonomic modulation or selective vagal denervation using RF ablation has been previously applied for patients with refractory vasovagal syncope. Pachon et al. reported that endocardial RF catheter ablation of severe neutrally meditated reflex syncope prevented pacemaker implantation and showed excellent long-term results in well selected patients [12]. The intrinsic cardiac autonomic nervous system (ANS) contains a network of autonomic ganglia and interconnecting neurons and axons. Even if one GP is denervated by RF ablation, the function of ANS may be compensated by other GPs. Hence, it is suggested that the reduction of compensatory ability among GPs induced by extensive ablation on multi-GP areas may lead to less recurrence.
In our study, HFS was used to localize the GP sites to minimize collateral myocardial damage and iatrogenic atrial tachycardias. During ablation, positive vagal response was more likely to occur in GP located at the SLGP, ARGP and SAGP. A larger sinus rate increase was more often seen after ablating these GPs, indicating that these GPs may play a more important role in controlling sinus rate. There are several limitations in our study. This treatment was performed in only one patient, and thus a larger number of patients should be treated and followed in randomized, blinded placebo-controlled trials, which is necessary to confirm the effect of this procedure in patients with long-standing SB. We have shown that autonomic denervation is effective during the 1-year follow-up period, but the long-term follow-up data of this procedure are still lacking.
Conclusion
Autonomic denervation in LA and RA by endocardial ablation of GP may increase sinus rate and improve symptoms in nonelderly patients with longstanding symptomatic SB. The approach demonstrates the feasibility from our early experience and may be offered as an alternative interventional treatment to a selective group of patients with longstanding symptomatic SB. Nonetheless, as rule for any new therapy the results must be confirmed with experimental protocols and by randomized studies.
Source of Funding
This study was supported by the Sponsored by Shanghai Sailing Program (No. 20YF1444300) and also supported by the National Key Research and Development Project (Grant Number 2018YFC1312503).
For More information: https://biomedgrid.com/fulltext/volume10/atrial-autonomic-denervation-for-the-treatment-of-longstanding-symptomatic-sinus-bradycardia-a-case-report.001523.php
Know More Information: Biomed Grid Please Click on : https://biomedgrid.com
For More information: Open Access Journals of Biomedical Science and Research: Journal of Biomedical Science
Know More Information: Biomed Grid Please Click on : https://biomedgrid.com

Comments
Post a Comment